If care is not moved out of hospitals and closer to people’s homes then the equivalent of around half the population will be visiting A&E every year by 2034, England’s top doctor has warned.
Professor Sir Stephen Powis, NHS England’s national medical director, said that if the NHS is to “avoid a situation of overcrowded A&Es” in a decade’s time then it must “go for broke” in moving care from hospital to the community.
A&Es around the country have reported extreme pressure in recent weeks, with many declaring critical incidents coupled with distressing reports about the care patients have received.
In a keynote speech on “The current state of the NHS” at Liverpool Medical Institution on Wednesday evening, Sir Stephen is expected to say: “I want to particularly focus today on moving care into the community.
“Because we know that if A&E attendances increase at the same rate as they have over the past 10 years – NHS staff will need to manage six million more A&E attendances every year from 2034.
“That would mean the equivalent of almost half the population attend A&E at least once every year – that is simply not feasible for a 21st-century health system.
“Instead, millions of patients will need to receive the care and support they need outside of hospital.
“The NHS is already on the right track in delivering this – whether in the rollout of high-tech virtual wards or two-hour urgent community response teams.”
A&Es in England faced the busiest year on record in 2024, with 27.42 million attendances across the year – 7.1% higher than in 2023, according to NHS England.
Rough projections suggest there could be 33,505,330 attendances in 2034.
Sir Stephen will address medical students, doctors and recently retired and will urge them to engage in the 10-year health plan.
We need your consent to load this Social Media content. We use a number of different Social Media outlets to manage extra content that can set cookies on your device and collect data about your activity.
“If the NHS is to avoid a situation of overcrowded A&Es in 10 years’ time – we must go for broke in moving care from hospital to the community,” he is expected to add.
“The mechanism for how we do that is still up for discussion.
“So as doctors of the past, present and future – we need your experience and expertise to support us to go further and faster.
“I urge everyone in this room to come forward with your experiences of what is and isn’t working in the NHS – so we can make the best practice, normal practice across the country as part of the 10-Year Health Plan,” he will add.
(PA Graphics)
Health Secretary Wes Streeting has invited patients and NHS staff to take part in a “national conversation” to shape the plan, a central plank of Labour’s health policy.
The party has pledged to build “an NHS fit for the future”, with a greater emphasis on preventing ill health, shifting care from hospitals to the community and harnessing the latest technology to improve care.
Sir Stephen’s comments come after a report last week found patients are dying in corridors and sometimes going undiscovered for hours, while sick people are being left to soil themselves.
We need your consent to load this Social Media content. We use a number of different Social Media outlets to manage extra content that can set cookies on your device and collect data about your activity.
The Royal College of Nursing (RCN) report, which has been described as “harrowing”, told of patients sitting for days in chairs – so-called “chair care” – people left in corridors, delays to treatment and the elderly unable to get help because of a lack of call bells and not enough staff.
The RCN found patients are regularly treated in bathrooms, shower areas, cloakrooms, bereavement rooms and even viewing rooms where families visit dead relatives.
It has also called for immediate Government action to end “corridor care”, which it says has become normalised and is not just occurring in the winter months.
Leading doctors from the Royal College of Physicians (RCP) have echoed concerns, saying there should be a “zero tolerance” approach to NHS corridor care.
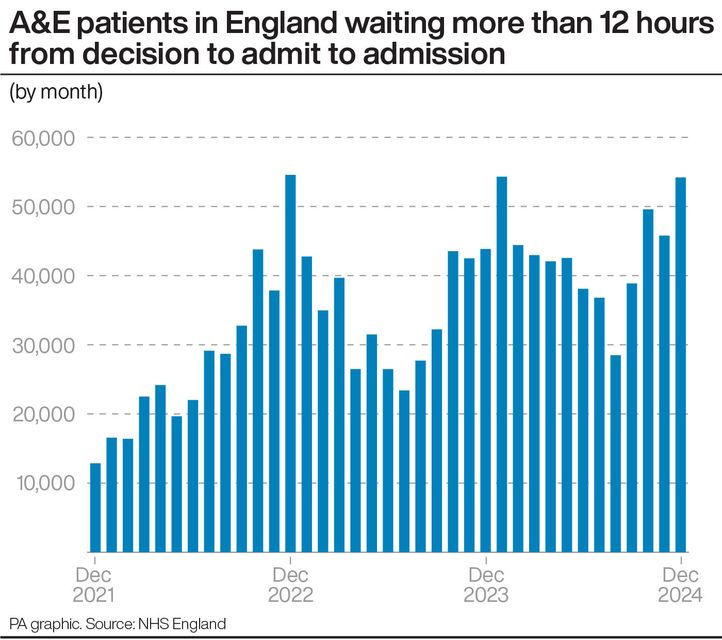
In December, more than 54,000 patients in England waited more than 12 hours for admission to a bed, while research shows that patients who spend more than 12 hours in A&E are twice as likely to die within 30 days as those dealt with within two hours.