An ombudsman’s inquiry into the death of a prisoner in custody has recommended the Health Trust change how it treats and diagnoses patients presenting with chest pain.
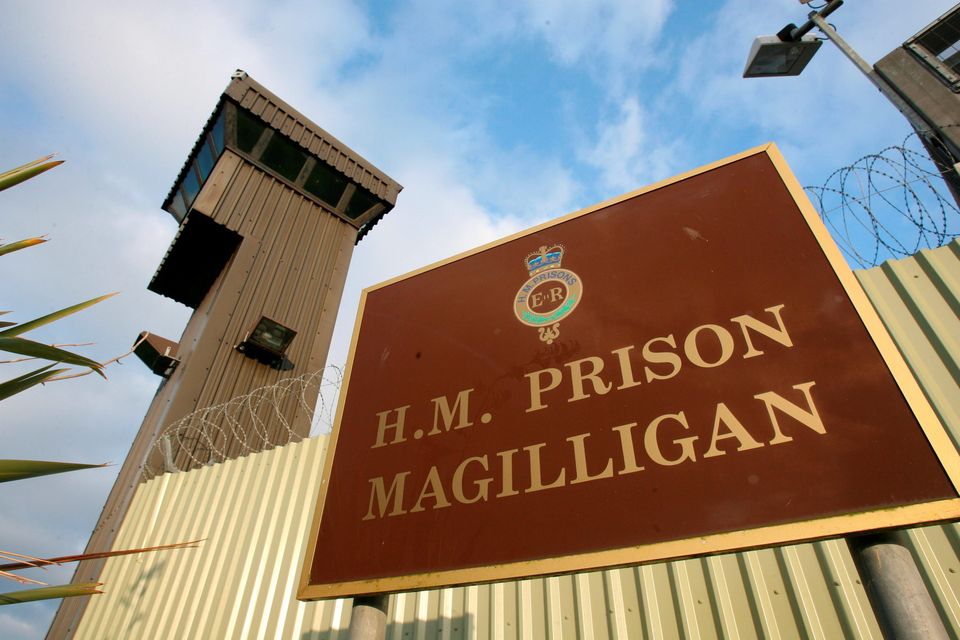
Mr ‘T’, not his real name and 64 years old, died in hospital in November 2018 after developing heart problems in HMP Magilligan in Co Londonderry.
The Prison Ombudsman’s report has found that while he received the same level of care he would have done in the community, the Trust can improve how it manages patients with chest pain and should ensure certain tests are overseen by specialist doctors.
The report has been signed off by current Ombudsman Jacqui Durkin, who notes that it was “at an advanced stage” when the previous ombudsman Dr Lesley Carroll left the role in February of this year.
Mr T began his time in custody in Maghaberry in October 2013, before being transferred to Magillgan prison in May 2016.
During his time in prison, Mr T worked as an orderly while also taking part in educational programmes. He was part of a progressive release and earned privileges schemes.
Read more
Mr T was noted as being a long-term smoker and had a history of mental ill health and self-harm.
Around October 2018, a fellow prisoner and close friend of his had recently passed away in custody.
Mr T’s cardiac problems were first reported on November 23, 2018, when he told a treatment room nurse in Magilligan that he was experiencing shortness of breath when exerting himself.
Later that day, he returned “distressed and clutching his chest”, complaining of severe tightness.
After receiving an ECG, a doctor prescribed him a Glyceryl Trinitrate (GTN) spray. NHS UK describes a GTN spray as a “nitrate” that is “used to prevent and treat chest pain caused by angina”.
He stayed under observation and received check-ups until November 27 when a nurse and doctor advised he attend A&E.
A junior locum doctor there checked on him before discharging him, scheduling an appointment with the chest pain clinic for two weeks later.
Mr T had been in Magilligan since 2016.
The ombudsman agreed with a clinical reviewer, who raised concerns with how Mr T was treated in A&E.
Mr T was still experiencing chest pains on November 28 and was “very worried about himself.” He had to cancel an Unaccompanied Temporary Release he had scheduled for that day.
Because he was now experiencing chest pains “while at rest”, a nurse strongly advised him to attend A&E, wanting to send for an ambulance. She “explained the consequences of what could happen if he refused to attend hospital”.
Mr T did not want to attend hospital, or get in an ambulance, and so was kept under close observation. Later that day, he reported feeling “fine” and having no further chest pains.
His health worsened dramatically on November 30, when a nurse was called to his room at 9:38am as he was experiencing chest pains.
There was a “sudden deterioration” in his health around 11:24, and an ambulance was called for.
He arrived at Altnagelvin A&E at 12.38pm, and by 1.34pm, doctors had to try and resuscitate him. They were unable to do so, and he was declared dead at 1.46pm.
The Ombudsman concurred with the opinion of clinical reviewers, that an ambulance should have been called at 9/9.30am on the day of his death, but that this was unlikely to have made a difference to the outcome as he was likely “already verging on cardiogenic shock”.
The report makes three recommendations. Firstly, after finding Mr T should’ve been prescribed additional medications on November 23, that the Trust “should develop pathways for the management of patient’s chest pain that includes the potential prescription of anti-ischaemic medication and antiplatelet drugs by doctors”.
Secondly, after finding that there were “subtle changes” in an ECG performed on November 28 that an expert doctor would’ve picked up on, that the Trust “should ensure that staff carrying out ECGs have access to timely interpretation from trained staff such as a doctor who is on or off site or an appropriately trained nurse”.
Thirdly, the report says the Trust should consider recommending all men in custody “regularly avail” of health checks, including “blood pressure measurement, smoking and diet advice and fasting lipid tests”.
The Ombudsman thanked Mr T’s family for their help in the investigation and shared condolences.
The Ombudsman also acknowledged “the length of time it has taken to complete the investigation and this report.”
“I appreciate the patience and continued engagement of Mr T’s family and am grateful to them for their contribution to this investigation.”